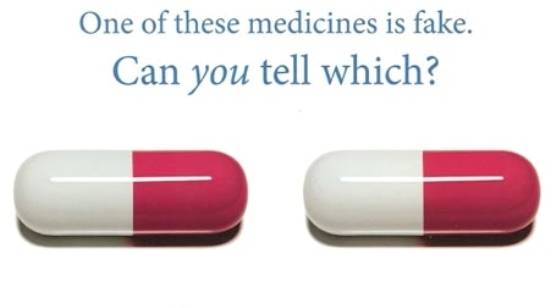
Poor-quality medicines pose a serious public health problem. The vested interests make every possible effort to make availability of deliberately falsified and substandard medicines in the market and because of the poor manufacturing and quality-control practices in the production of genuine drugs; these medicines reach patients abundantly and conveniently. Substandard medicines continue to be present in almost all of the states in the world, but with varying quantities, which display a great threat to health because they can carelessly lead to healthcare failures such as antibiotic resistance and the spread of diseases in a society as well as deaths or additional illnesses in individuals. The grave state of affairs necessitates some innovative reforms.
Shockingly, not unlike some other WHO member countries, Pakistan faces the illegitimate but lucrative trade of counterfeit and substandard drugs to the epidemic proportions. As most of the pharmaceutical industry in the country is unregulated with hardly checks or balances in place, therefore a great number of pharmaceutical companies producing and supplying spurious and substandard medicines have been endangering unaccounted innocent lives, particularly in rural regions of the country.
According to the World Health Organization (WHO), each pharmaceutical product that a manufacturer produces has to comply with quality standards and specifications at release and throughout the product shelf-life required by the territory of use. Normally, these standards and specifications are reviewed, assessed and approved by the relevant national medicines regulatory authority (NMRA) before the product is authorized for marketing. Substandard medicines are pharmaceutical products that do not meet their quality standards and specifications.
The WHO estimates that only approximately 20% of its 191 member states have well-developed drug regulation; around 30% are thought to have no or minimal drug regulation in place. Alarmingly, in Pakistan the pharmaceutical industry has been operating without formal control since the national Ministry of Health was abolished in June 2011 and its power devolved to the provinces. However, following the deaths in January 2012 of 120 patients in Lahore due to substandard heart medicines,the government of Pakistan established the Drug Regulatory Authority to regulate the country's pharmaceutical industry. The authority has yet no shown fruitful results because even today hundreds of unregulated pharmaceutical companies exist in the country especially in Punjab and Sindh provinces which are the cause of great concern for millions of people.
Reportedly substandard medicines are ineffective but their use leave a number of hazardous side effects on the users’ health. Despite the fact that patients take doses of medicines continuously for a long time as prescribed by doctors for various illnesses but there is no improvement in their health condition. Moreover, patients suffering from headache, fever, stomach pain and malaria take medicines particularly antibiotic ones, which give them relief from these diseases but affect their vital bodily organs such as heart, liver, kidney, and brain badly. As a result, the patients instead of becoming healthy get seriously ill.
Doctors can also be blamed for flourishing trade of substandard medicines because they play a significant role in this dirty business. Marketing incentives and strategies used by both multinational and national pharmaceutical companies often convince doctors to prescribe non-generic and/or over-priced drugs. Many of the patients do not have the knowledge to gauge the quality of medicines. They rely on either the doctor or the pharmacist for such information. And the misconception has been created amongst the people in our society that the more expensive the drug, the more effective it will be, which has helped the dishonest elements producing counterfeit drugs in further increasing their profit margins.
Although healthcare is a serious issue yet the quality of medicines is not ensured in most of the government run hospitals for the proper treatment of various diseases across the country. Reportedly, the government hospitals continue to purchase spurious and substandard medicines from unregistered pharmaceutical companies without even getting them tested from laboratories whether the drugs are patient-friendly and up to the proper health standards or not. Consequently, the lives of millions of poor patients in these government hospitals are endangered due to non-availability of original and effective medicines.
Nigeria's National Agency for Food and Drug Administration (NAFDAC) has provided a model for how to improve the provision of safe medicines. It implemented a series of measures to combat falsified and poor-quality drugs and to ensure drug safety. According to a survey estimates, 68 percent drugs available in Nigeria in 2001 were unregistered which the NAFDAC registered 80 percent of them by 2004. The NAFDAC raised public awareness of falsified drugs publishing lists of identified fake/substandard products in newspapers after it brought about some inevitable and administrative developments. After all, the NAFDAC, in partnership with some pharmaceutical companies, order to ensure accessibility of only genuine drugs to the consumers, had also tested and adopted an innovative new mobile authentication service developed by a US company (Sproxil). The process of authentication is very easy, quick and interestingly free of cost for consumers. This includes a scratch panel is added to the drug package; the consumer reveals a code scratching it, which is sent in a text message to the authentication service. After confirming whether drug is fake or genuine, a message is sent back. India and Kenya have adopted the system.
To tackle the problem of substandard or counterfeit drugs before this cancer becomes even more deeply entrenched, the Drug Regulatory Authority of Pakistan in coordination with provincial health departments in order to eradicate the menace from the country should ensure accessibility, availability, appropriateness and the quality of goods and services. For this purpose, the DRA following in the footsteps of the NAFDAC should introduce authentication service after registering all of the unregistered drugs and setting on fire already produced falsified medicines.